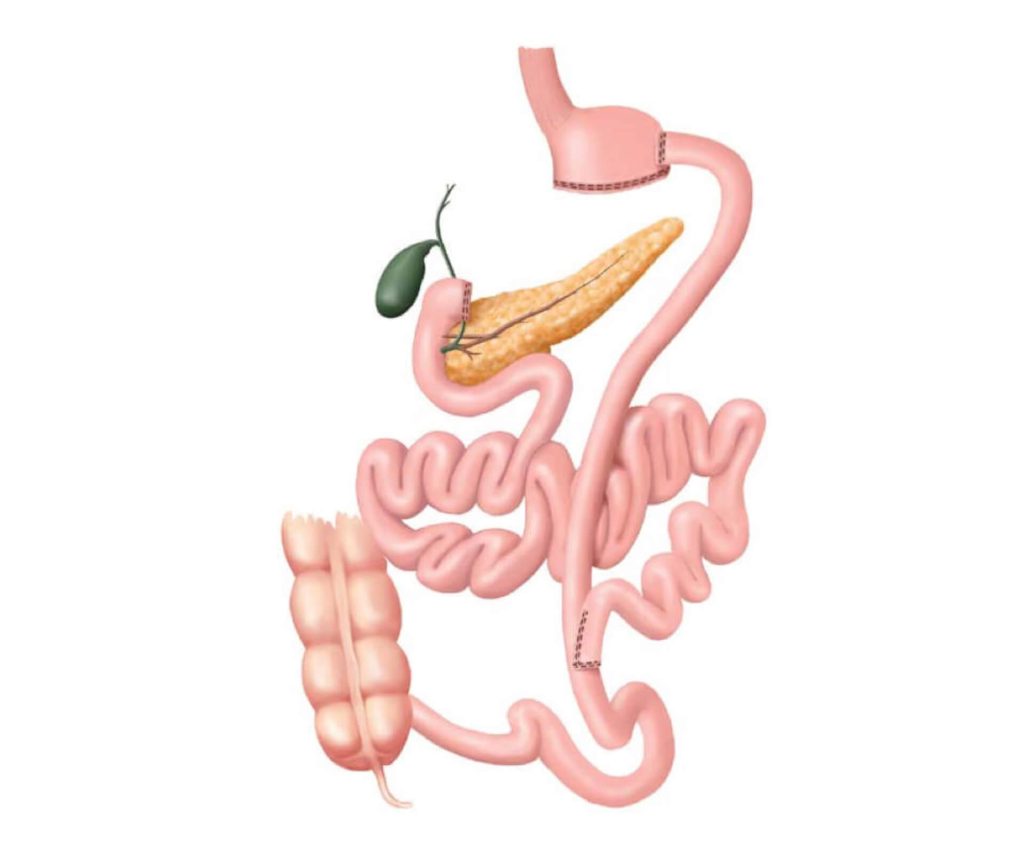
Gastrointestinal operations, originally used to treat severe obesity (“bariatric” or “weight-loss surgery”) cause rapid reversal of type 2 diabetes (disease remission) in many patients.
For a long-time this effect has been considered a consequence of weight loss; however, experimental studies in the early 2000s, pioneered by Francesco Rubino and colleagues demonstrated that gastrointestinal surgery has direct effects on diabetes, independent of weight loss.
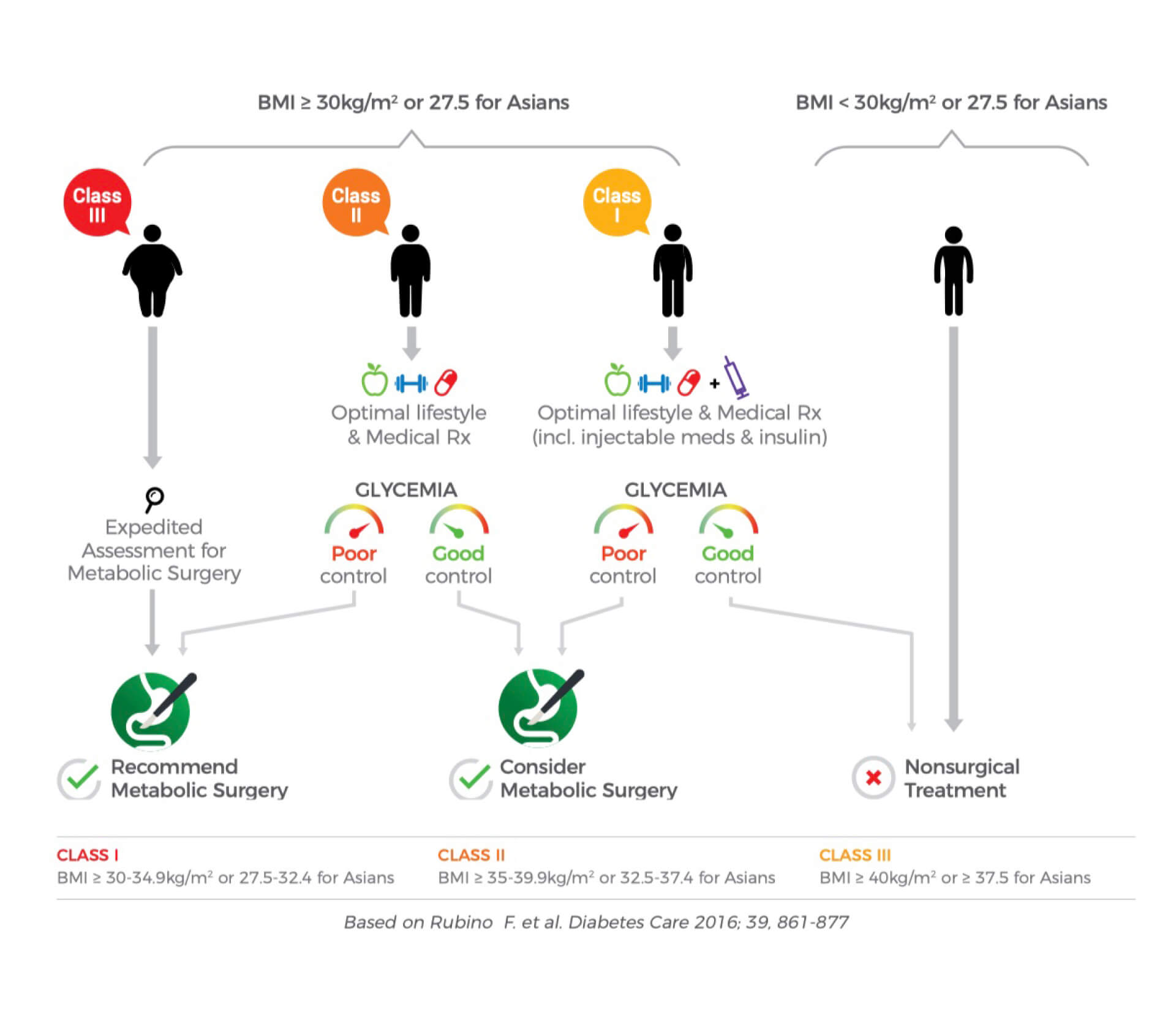
This finding provided a biological rationale to repurpose gastrointestinal operations and bariatric surgery as an intentional treatment of type 2 diabetes itself, a practice now referred to as “metabolic surgery”.